1822
Augustus Frederick d'Este (1794–1848), son of Prince Augustus Frederick, Duke of Sussex and Lady Augusta Murray and a grandson of George III of the United Kingdom, almost certainly had MS. D'Este left a detailed diary describing his 22 years living with the disease. His diary began in 1822 and ended in 1846, although it remained unknown until 1948. His symptoms began at age 28 with a sudden transient visual loss (amaurosis fugax) after the funeral of a friend. During his disease, he developed weakness in the legs, clumsiness of the hands, numbness, dizziness, bladder disturbance and erectile dysfunction. In 1844, he began to use a wheelchair. Despite his illness, he kept an optimistic view of life. Another early account of MS was kept by the British diarist W. N. P. Barbellion, pen name of Bruce Frederick Cummings (1889–1919), who maintained a detailed log of his diagnosis and struggle. His diary was published in 1919 as The Journal of a Disappointed Man. Charles Dickens, a keen observer, described possible bilateral optic neuritis with reduced contrast vision and Uhthoff's phenomenon in the main female character of Bleak House (1852–1853), Esther Summerson.
1863
Robert Carswell (1793–1857), a British professor of pathology, and Jean Cruveilhier (1791–1873), a French professor of pathologic anatomy, described and illustrated many of the disease's clinical details, but did not identify it as a separate disease. Specifically, Carswell described the injuries he found as "a remarkable lesion of the spinal cord accompanied with atrophy". Under the microscope, Swiss pathologist Georg Eduard Rindfleisch (1836–1908) noted in 1863 that the inflammation-associated lesions were distributed around blood vessels.
1868
MS was first described in 1868 by French neurologist Jean-Martin Charcot. The name "multiple sclerosis" is short for multiple cerebro-spinal sclerosis, which refers to the numerous glial scars (or sclerae – essentially plaques or lesions) that develop on the white matter of the brain and spinal cord.
1868
The French neurologist Jean-Martin Charcot (1825–1893) was the first person to recognize multiple sclerosis as a distinct disease in 1868. Summarizing previous reports and adding his own clinical and pathological observations, Charcot called the disease sclerose en plaques.
1868
The first attempt to establish a set of diagnostic criteria was also due to Charcot in 1868. He published what now is known as the "Charcot triad", consisting of nystagmus, intention tremor, and telegraphic speech (scanning speech). Charcot also observed cognition changes, describing his patients as having a "marked enfeeblement of the memory" and "conceptions that formed slowly".
1965
The diagnosis was based on Charcot triad and clinical observation until Schumacher made the first attempt to standardize criteria in 1965 by introducing some fundamental requirements: Dissemination of the lesions in time (DIT) and space (DIS), and that "signs and symptoms cannot be explained better by another disease process". The DIT and DIS requirement was later inherited by the Poser and McDonald criteria, whose 2017 revision is in use.
1996
In 1996, the US National Multiple Sclerosis Society (NMSS) (Advisory Committee on Clinical Trials) defined the first version of the clinical phenotypes that is in use. In this first version, they provided standardized definitions for four MS clinical courses: relapsing-remitting (RR), secondary progressive (SP), primary progressive (PP), and progressive relapsing (PR). In 2010, PR was dropped and CIS was incorporated. Three years later, the 2013 revision of the "phenotypes for the disease course" were forced to consider CIS as one of the phenotypes of MS, making obsolete some expressions like "conversion from CIS to MS". Other organizations have proposed later new clinical phenotypes, like HAMS (Highly Active MS).
2010
A 2022 Cochrane review found that nabiximols (a specific Cannabis extract first approved in the United Kingdom in 2010) likely reduces the severity of spasticity as an adjunctive therapy to standard anti-spasticity medication in the short term, but may have increased medication discontinuation to a small degree due to adverse events.
2011
In 2011, mitoxantrone was the first medication approved for secondary progressive MS. In this population, tentative evidence supports mitoxantrone moderately slowing the progression of the disease and decreasing rates of relapses over two years.
2013
The International Advisory Committee on Clinical Trials of MS describes four types of MS (revised in 2013) in what is known as the Lublin classification:
March 2017
New approved medications continue to emerge. In March 2017, the FDA approved ocrelizumab as a treatment for primary progressive MS in adults, the first drug to gain that approval, with requirements for several Phase IV clinical trials. It is also used for the treatment of relapsing forms of multiple sclerosis, to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease in adults. According to a 2021 Cochrane review, ocrelizumab may reduce worsening of symptoms for primary progressive MS and probably increases unwanted effects but makes little or no difference to the number of serious unwanted effects.
2019
In 2019, siponimod and cladribine were approved in the United States for the treatment of secondary progressive multiple sclerosis (SPMS). Subsequently, ozanimod was approved in 2020, and ponesimod was approved in 2021, which were both approved for management of CIS, relapsing MS, and SPMS in the U.S., and RRMS in Europe.
2020
MS is the most common immune-mediated disorder affecting the central nervous system (CNS). In 2020, about 2.8 million people were affected by MS globally, with rates varying widely in different regions and among different populations. The disease usually begins between the ages of 20 and 40 and is almost three times more common in females than in males (3:1 ratio).
December 2022
Ublituximab was approved for medical use in the United States in December 2022.
2024
In 2024, scientists shared research on their findings of ancient migration to northern Europe from the Yamnaya area of culture, tracing MS-risk gene variants dating back around 5,000 years. The MS-risk gene variants protected ancient cattle herders from animal diseases, but modern lifestyles, diets and better hygiene, have allowed the gene to develop, resulting in the higher risk of MS today.
September 2024
Ocrelizumab/hyaluronidase was approved for medical use in the United States in September 2024.
Trending
3 months ago Islanders face Rangers in first derby; betting promos available for the game.

Sha'Carri Richardson is a celebrated American track and field sprinter specializing in the and metres Her prominence surged in while...

7 months ago John Wall's NBA Return Celebrated, DeMarcus Cousins Adds Humor, Fans Show Love.
Jessica Tarlov is an American political strategist affiliated with the Democratic Party She is a co-host on the Fox News...

2 months ago Michelle Obama: America 'not ready' for a woman president, cites sexism concerns.
Vostok launched on April marked a pivotal moment in space exploration as the first human orbital spaceflight Aboard the Vostok...
Popular

Thomas Douglas Homan is an American law enforcement officer who...

William Franklin Graham III commonly known as Franklin Graham is...
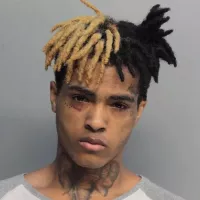
XXXTentacion born Jahseh Dwayne Ricardo Onfroy was a controversial yet...

Jupiter is the fifth and largest planet from the Sun...

Kristi Noem is an American politician who has served as...

Instagram is a photo and video-sharing social networking service owned...