COVID-19 testing is essential for identifying SARS-CoV-2 infections and tracking the pandemic. Two primary types exist: molecular tests detect the virus itself, aiding diagnosis and outbreak control. Antibody tests reveal past infections and help assess disease prevalence. Molecular tests are useful for the prompt diagnosis of individual cases of disease to contain spread by quarantining infected individuals. Antibody tests are not useful for diagnosis, but for evaluating how widespread the disease has been.
2000: False positives rate in rapid antigen tests
In a study of over 900,000 rapid antigen tests, false positives were found to occur at a rate of 0.05% or 1 in 2000.
2003: Nasal and throat swabs less suitable for diagnosis of SARS
In 2003, during the SARS outbreak, Drosten et al. noted that nasal and throat swabs were less suitable for diagnosis compared to sputum, as they contained less viral RNA, potentially leading to missed detections.
May 2015: Korea's MERS quarantine failure
The failure of Korea's MERS quarantine in May 2015 left Korea more prepared for COVID-19 than countries that did not face that pandemic.
2016: Korea allowed private sector testing for infectious diseases
In 2016, then President Park Geun-hye allowed Korean CDC-approved private sector testing for infectious diseases.
January 2020: First genetic sequences of SARS-CoV-2 published
In January 2020, scientists from China published the first genetic sequences of SARS-CoV-2 via virological.org.
April 2020: Antigen tests as a way to scale up testing
In April 2020, Deborah Birx of the White House Coronavirus Task Force suggested that antigen tests might be a way to scale up testing to much greater levels, since RT-PCR tests require too much time, energy and trained personnel to run the tests. She noted that it would not be possible to test everybody before they go to work or to school with PCR tests, but it might be possible with the antigen test.
April 2020: Paul Romer on Scaling Up Testing Capacity
In April 2020, Economist Paul Romer reported that the US has the technical capacity to scale up to 20 million tests per day to fully remobilize the economy.
May 2020: Probability of false-negative PCR-RT test results
In May 2020, a review of PCR-RT testing found that the median probability of a false-negative result decreased from 100% on day 1 to 67% on day 4. On the day of symptom onset, the probability was 38%, which decreased to 20% 3 days later.
July 2020: Fauci on RT-PCR tests cycle thresholds
In July 2020, Anthony Fauci of the US NIH indicated that positive results obtained from RT-PCR tests run at more than 35 cycles were almost always "just dead nucleotides".
July 2020: Estimated capacity to scale to 20 million tests per day by late July 2020
The Edmond J. Safra Center for Ethics estimated on April 4, 2020, that the capacity to scale up to 20 million tests per day could be available by late July 2020.
August 2020: WHO recognizes wastewater surveillance of SARS-CoV-2
As of August 2020, the WHO recognizes wastewater surveillance of SARS-CoV-2 as a potentially useful source of information on the prevalence and temporal trends of COVID-19 in communities.
August 2020: Cycle thresholds for testing data compiled by officials in Massachusetts, New York and Nevada
In August 2020, it was reported that in three sets of testing data that include cycle thresholds, compiled by officials in Massachusetts, New York and Nevada most tests set the limit at 40 cycles, a few at 37. The CDC was examining the use of cycle threshold measures for policy decisions.
August 2020: FDA Authorizes Yale Saliva Test
In August 2020, the US FDA granted emergency use authorization for a saliva test developed at Yale University that gives results in hours.
October 2020: Mass testing in Slovakia
In October 2020 Slovakia tested 3.62 million people in a weekend, from a population of 5.4m. 38,359 tested positive.
October 2020: Snapshot Mass-Testing Approach in Slovakia
In Slovakia, at the end of October 2020, approximately 80% of the population was tested for COVID-19 within a weekend. A study found that the snapshot mass-testing approach was highly efficacious, decreasing observed prevalence by 58% within one week and by 70% compared to a hypothetical scenario of no snapshot mass-testing.
2020: Warnings about Chinese-made testing kits in Nevada
In 2020, Nevada received a donation of 250,000 Covid testing kits from China's BGI Group. However, the US Department of Homeland Security and the State Department raised a warning for Nevada hospitals to not use the Chinese-made testing kits, as there were concerns around the involvement of the Chinese government, test accuracy and privacy of the patients.
2020: Accuracy dropped significantly when screening was conducted by the public instead of by a medical professional
In 2020, a study found 79% of positive cases were found when the Innova SARS-CoV-2 Antigen Rapid Qualitative Test was used by laboratory scientists, but only 58% when used by the general public and 40% when used for city-wide screening in Liverpool.
January 2021: Denmark suspended Emirati flights
In January 2021, the COVID-19 testing results of the UAE came under scrutiny, as Denmark suspended the Emirati flights for five days. The European nation said that it barred the flights from the UAE due to growing suspicion of irregularities in the testing process being followed in the Gulf nation.
January 2021: FDA Alert on False Results with Curative SARS-Cov-2 Assay
In January 2021, the US FDA issued an alert about the risk of false results, particularly false negative results, with the Curative SARS-Cov-2 Assay real-time RT-PCR test.
April 2021: Innova SARS-CoV-2 Antigen Rapid Qualitative Test recall
In April 2021, The FDA inspected Innova facilities in California and found inadequate quality assurance of tests manufactured in China. On 23 April 2021, the company issued a recall for the Innova SARS-CoV-2 Antigen Rapid Qualitative Test.
May 2021: Bees and Dogs Detection of COVID-19
In May 2021, Reuters reported that Dutch researchers at Wageningen University had shown that trained bees could detect the virus in infected samples in seconds. Also in May 2021, a study reported that dogs were more reliable than current lateral flow tests.
July 2021: CDC on tests results determined at 40 cycles
On July 21, 2021, the CDC indicated tests results should be determined at 40 cycles.
August 2021: Exceptional use authorization for Innova SARS-CoV-2 Antigen Rapid Qualitative Test until August 28, 2021
As of August 2021, over 1 billion Innova SARS-CoV-2 Antigen Rapid Qualitative Tests from the company have been distributed in the UK, with £3 billion in funding as part of Operation Moonshot, and the MHRK has authorized exceptional use until at least 28 August 2021.
2021: Molecular tests for virus detection
As of 2021, the most common form of molecular test is the reverse transcription polymerase chain reaction (RT-PCR) test. Nucleic acid or molecular tests detect the presence of the virus's RNA. Other methods used in molecular tests include CRISPR, isothermal nucleic acid amplification, digital polymerase chain reaction, microarray analysis, and next-generation sequencing in 2021.
March 2022: Dogs can effectively detect SARS-Cov2 in people
In March 2022, Researchers in Paris reported that trained dogs were very effective for rapidly detecting the presence of SARS-Cov2 in people, whether displaying symptoms or not. The dogs were presented with sweat samples to smell from 335 people, of whom 78 with symptoms and 31 without tested positive by PCR. The dogs detected 97% of the symptomatic and 100% of the asymptomatic infections.
2023: At-home COVID-19 tests mailed to households
In 2023, in Hong Kong test subjects could stay home and receive a specimen tube. They spit into it, return it and later get the result. Additionally, by the fall of 2023, the United States had conducted six rounds of mailing free at-home COVID-19 tests to households nationwide.
Mentioned in this timeline

Anthony Stephen Fauci is a prominent American physician-scientist and immunologist...

The White House located at Pennsylvania Avenue NW in Washington...
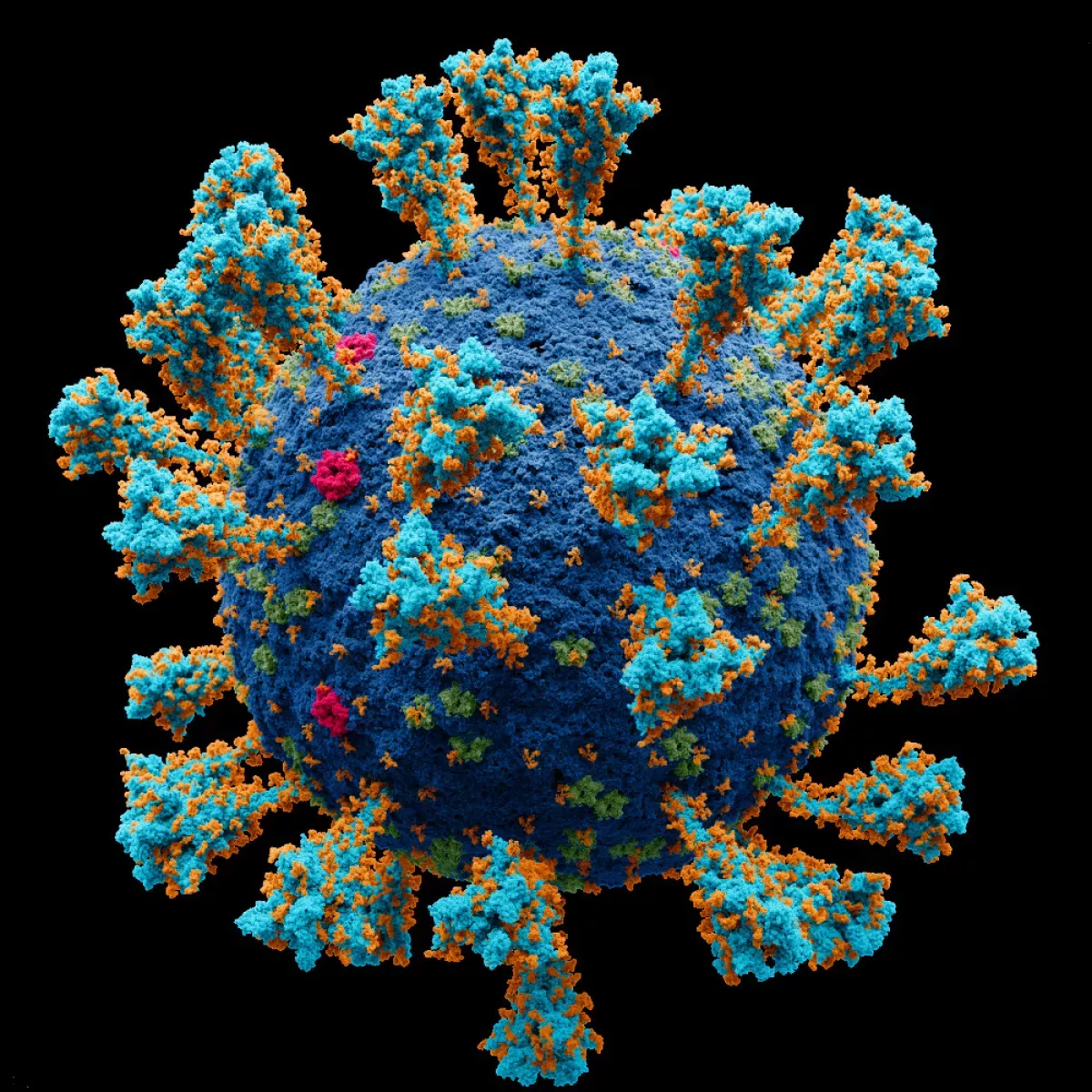
Coronaviruses are a family of RNA viruses affecting mammals and...
Hong Kong is a densely populated special administrative region of...
China officially the People's Republic of China is an East...
Korea is a peninsular region in East Asia comprised of...
Trending

36 minutes ago Kris Dunn Shines: Steals the Show with Impressive Defensive Performance for Clippers

36 minutes ago Queta's Hilarious Clip Evokes Mazzulla Memories: A Lighthearted NBA Moment
36 minutes ago Howard Lutnick faces potential subpoena in Epstein investigation, House Republicans consider deposition.

36 minutes ago Nakashima at Acapulco Open 2026: Match Predictions and Results Analysis.

37 minutes ago Donte DiVincenzo's Underrated Impact on Timberwolves: A Deep Dive into His Contributions

37 minutes ago Luka Don?i?'s Botched Play and Sam Mitchell's Criticism Doom Lakers Against Magic
Popular

Jesse Jackson is an American civil rights activist politician and...

Susan Rice is an American diplomat and public official prominent...

Barack Obama the th U S President - was the...
XXXTentacion born Jahseh Dwayne Ricardo Onfroy was a controversial yet...

Michael Joseph Jackson the King of Pop was a highly...

Kashyap Pramod Patel is an American lawyer who became the...