1944: Lipopolysaccharide Character of Endotoxins Determined
The lipopolysaccharide nature of enteric endotoxins, which are substances produced by bacteria that can cause harmful effects in the body, was established by Shear in 1944.
1965: Discovery of Endotoxin-Resistant Mice
A strain of C3H/HeJ mice that displayed immunity to endotoxin-induced shock was identified in 1965.
1973: Molecular Structure of Endotoxins Revealed
Luderitz and colleagues elucidated the detailed molecular structure of endotoxins in 1973.
1979: Sepsis Incidence Begins to Rise
From 1979 to 2000, data from the United States National Hospital Discharge Survey indicated a fourfold increase in the incidence of sepsis, reaching 240 cases per 100,000 people.
1997: Sepsis Costs Quadruple Since 1997
From 1997 to 2013, the cost of sepsis hospital stays in the United States increased more than fourfold, with an average annual increase of 11.5%.
1998: Toll-Like Receptor 4 Identified
The discovery of the toll-like receptor gene 4 (TLR4) in 1998 established a connection between this gene and the observed resistance to lipopolysaccharide in certain mice strains.
2000: Decline in Sepsis Case Fatality Rate
Between 1979 and 2000, there was a reduction in the in-hospital case fatality rate associated with sepsis, dropping from 28% to 18%.
2002: Establishment of the Surviving Sepsis Campaign
An international collaborative effort called the "Surviving Sepsis Campaign" was launched with the goal of educating the public about sepsis and enhancing patient outcomes. The campaign released an evidence-based assessment of severe sepsis management approaches, intending to provide a comprehensive set of recommendations in the following years.
2003: Severe Sepsis Cases Increase in the U.S.
According to the nationwide inpatient sample from the United States, the occurrence of severe sepsis rose from 200 cases per 10,000 individuals in 2003 to 300 cases by 2007 among those over 18 years old.
2007: Severe Sepsis Incidence Continues to Climb
By 2007, the incidence of severe sepsis had reached 300 cases per 10,000 individuals over the age of 18 in the United States.
2010: Sepsis Hospitalization Rate in the U.S.
In 2010, there were approximately 651 hospital stays for every 100,000 people in the United States due to a sepsis diagnosis.
2011: Sepsis as a Leading Cause of Hospital Readmission
In 2011, a study covering 18 U.S. states revealed that sepsis was the second most frequent primary reason for hospital readmission within a 30-day period among Medicare beneficiaries.
2011: Recombinant Activated Protein C Withdrawn from Market
Recombinant activated protein C (drotrecogin alpha) was initially used for severe sepsis but subsequent studies revealed that it increased adverse events, particularly bleeding risk, without reducing mortality, leading to its withdrawal from the market in 2011.
2012: Cochrane Review Finds N-acetylcysteine Ineffective for SIRS and Sepsis
A Cochrane review from 2012 concluded that N-acetylcysteine does not improve mortality rates in individuals with systemic inflammatory response syndrome (SIRS) or sepsis, and it might even have harmful effects.
2012: SuPAR as a Prognostic Marker, Not a Diagnostic Tool, for Sepsis
A systematic review determined that soluble urokinase-type plasminogen activator receptor (SuPAR), while not an accurate diagnostic marker for sepsis, held prognostic value. Elevated SuPAR levels correlated with a higher mortality risk in sepsis patients.
2013: Procalcitonin as a Diagnostic Marker for Sepsis
A review found moderate evidence supporting the use of procalcitonin levels to differentiate sepsis from non-infectious causes of SIRS. While helpful, procalcitonin levels alone were not considered definitive for diagnosis.
2013: Controversy over Mouse Models in Sepsis Research
A scientific controversy emerged regarding the use of mouse models in sepsis research. A review highlighted significant differences between mouse and human immune systems, questioning the validity of mouse models. This review revealed that numerous human sepsis trials, supported by promising mouse data, had failed. Consequently, some researchers advocated for abandoning mouse models in sepsis research, while others urged caution in interpreting mouse study results and emphasized meticulous preclinical study design. One proposed approach involved prioritizing the study of biopsies and clinical data from sepsis patients to identify biomarkers and drug targets.
2013: Sepsis as the Most Expensive Condition in US Hospitals
In 2013, sepsis became the most expensive condition treated in US hospitals, costing $23.6 billion for nearly 1.3 million hospitalizations.
2013: ICD-10 Replaces ICD-9 in the U.S.
The United States transitioned from using the International Statistical Classification of Diseases and Related Health Problems (ICD) version 9 to ICD-10 in 2013, leading to changes in terminology related to sepsis.
2014: Impact of Blood Transfusions on Sepsis Survival
A trial found that maintaining hemoglobin levels above 70 or 90 g/L through blood transfusions did not affect survival rates in sepsis patients. A lower transfusion threshold led to fewer total transfusions.
2016: Surviving Sepsis Campaign Recommends Tapering Steroids
The 2016 Surviving Sepsis Campaign recommended tapering off steroids when vasopressors are no longer needed.
2016: Surviving Sepsis Campaign Recommends Low-Dose Hydrocortisone
The 2016 Surviving Sepsis Campaign recommended using low-dose hydrocortisone only when intravenous fluids and vasopressors were insufficient to treat septic shock effectively.
2016: Surviving Sepsis Campaign Guideline Update
The Surviving Sepsis Campaign updated their guidelines for management of sepsis.
2016: Simplified Sepsis Diagnosis with qSOFA
The quick SOFA score (qSOFA) replaced the SIRS system for diagnosing sepsis. qSOFA uses three criteria: increased breathing rate, altered mental status, and low blood pressure. At least two of these criteria must be met for a sepsis diagnosis.
2016: SOFA and qSOFA Scores Replace SIRS for Sepsis Screening
The sequential organ failure assessment (SOFA) score and its abbreviated version (qSOFA) replaced the systemic inflammatory response syndrome (SIRS) for sepsis screening. qSOFA, designed for use outside the ICU, assesses respiratory rate, blood pressure, and mental status.
2017: Marik Protocol for Sepsis Prevention
Paul E. Marik introduced the "Marik protocol," also known as the "HAT" protocol, which proposed a combination of hydrocortisone, vitamin C, and thiamine as a sepsis prevention strategy for individuals in intensive care. Marik's initial research demonstrated significant benefits, leading to the protocol's popularity among intensive care physicians, particularly after gaining attention on social media and National Public Radio. However, the protocol faced criticism from the broader medical community due to concerns about science by press conference. Subsequent independent studies failed to replicate Marik's findings, raising the possibility of bias.
2017: Global Impact of Sepsis
Sepsis affected approximately 49 million people globally, leading to 11 million deaths, making it responsible for 1 in 5 deaths worldwide.
2019: Cochrane Review and Other Studies Evaluate Corticosteroid Use
A Cochrane Review conducted in 2019, along with two other reviews from the same year, found low-quality evidence supporting the benefits of using corticosteroids for sepsis treatment.
2021: Systematic Review of Marik Protocol
A systematic review conducted in 2021 found that the Marik protocol's purported benefits could not be substantiated. Another review noted that while HAT therapy appeared to significantly reduce the duration of vasopressor use and enhance the SOFA score, it did not demonstrate substantial benefits in other outcomes for sepsis patients.
2021: Uncertainty Regarding Vitamin C's Role in Sepsis Treatment
As of 2021, the evidence supporting the use of vitamin C in sepsis treatment remained inconclusive.
2021: Surviving Sepsis Campaign Guidelines Question qSOFA as a Single Screening Tool
The Surviving Sepsis Campaign advised against using qSOFA as the sole screening tool for sepsis or septic shock, recommending a combination of SIRS, NEWS, or MEWS for more comprehensive assessment.
2021: Surviving Sepsis Campaign Guideline Update
The Surviving Sepsis Campaign again updated their guidelines for management of sepsis.
2021: Surviving Sepsis Campaign Updates Recommendations on Corticosteroids
The Surviving Sepsis Campaign updated its guidelines in 2021 to recommend intravenous corticosteroids for adults experiencing septic shock who require ongoing vasopressor therapy.
Mentioned in this timeline

News encompasses information about current events disseminated through various media...
Trending
7 minutes ago 2026 Primary Elections: Updates from Texas House District 23 and North Carolina.
8 minutes ago Lamine Yamal Eclipses Ronaldo, Messi: Is Barcelona Too Dependent? Historic Performance Liberates

1 hour ago Malik Willis' Value Debated as Cardinals and Steelers Weigh Options in NFL.
1 hour ago Inter faces Como in Coppa Italia: Chivu makes eight changes in formation.
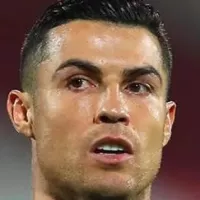
1 hour ago Cristiano Ronaldo suffers hamstring injury; Al Nassr confirms major blow for the star.

1 hour ago Raphinha becomes the new face of Calvin Klein's underwear campaign: Exclusive photos.
Popular

Jesse Jackson is an American civil rights activist politician and...

Hillary Diane Rodham Clinton is a prominent American politician lawyer...
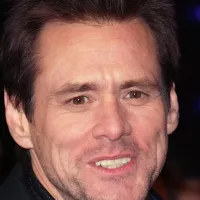
Jim Carrey is a Canadian-American actor and comedian celebrated for...
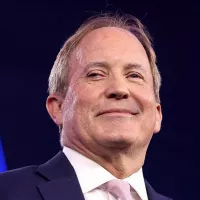
Ken Paxton is an American politician and lawyer serving as...
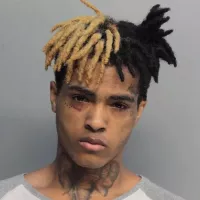
XXXTentacion born Jahseh Dwayne Ricardo Onfroy was a controversial yet...

Bill Clinton served as the nd U S President from...
