Endometriosis is a condition where tissue similar to the uterine lining (endometrium) grows outside the uterus. It commonly affects reproductive organs like ovaries and fallopian tubes, the uterus's outer surface, and surrounding tissues. However, it can also occur in other pelvic organs such as the bowels, bladder, or, rarely, distant body parts. Endometriosis is found in humans and some menstruating mammals.
1948: High-dose estrogen therapy
In 1948, High-dose estrogen therapy with diethylstilbestrol for endometriosis was first reported by Karnaky.
1971: Danazol for endometriosis
In 1971, Danazol was first described for endometriosis and became the main therapy in the 1970s and 1980s.
1996: Staging classification by ASRM
In 1996, Endometriosis can be classified as stage I–IV by the scale of the American Society of Reproductive Medicine (ASRM).
1996: Revision of the American Society of Reproductive Medicine's scale
In 1996, the American Society of Reproductive Medicine's scale was revised, giving higher scores to deep, thick lesions or intrusions on the ovaries and dense, enveloping adhesions on the ovaries or fallopian tubes.
2010: Biomarkers for endometriosis
In 2010, essentially all proposed biomarkers for endometriosis were of unclear medical use, although some appeared to be promising.
2011: Identification of putative biomarkers
Another review in 2011 identified several putative biomarkers upon biopsy, including findings of small sensory nerve fibers or defectively expressed β3 integrin subunit.
2013: Lack of knowledge among healthcare providers
Half of general health care providers surveyed in a 2013 study were unable to name three symptoms of endometriosis, showing a lack of knowledge among primary care physicians.
2015: Global estimate of affected people
One estimate is that 10.8 million people were affected globally by endometriosis as of 2015.
2016: Review of endometrial biomarkers
A 2016 review of endometrial biomarkers for diagnosing endometriosis was unable to draw conclusions due to the low quality of the evidence.
2017: Literature review on excision vs ablation
A 2017 literature review found that excision improved some outcomes over ablation in treating endometriosis.
2018: Swedish systematic review
A 2018 Swedish systematic review found a large number of studies but a general lack of scientific evidence for most endometriosis treatments.
2018: Oral GnRH antagonists introduced
Oral GnRH antagonists such as elagolix were introduced for the treatment of endometriosis in 2018.
2019: Genome-wide association study review
In 2019, a genome-wide association study (GWAS) review identified 36 genes with mutations associated with endometriosis development, with nine chromosome loci being robustly replicated.
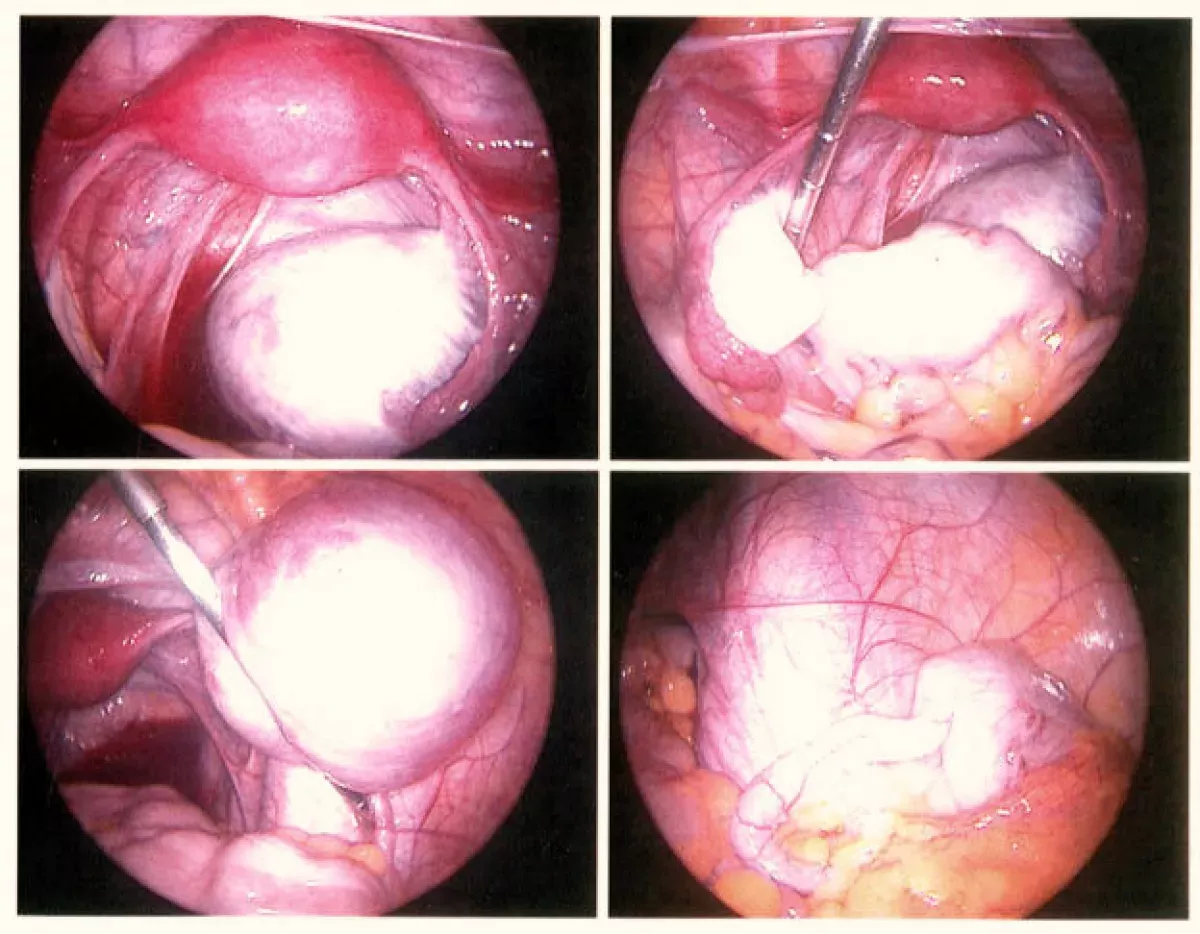
2019: Endometriosis diagnosis and laparoscopy
Reviews in 2019 concluded that advances in imaging meant endometriosis diagnosis should no longer be considered synonymous with immediate laparoscopy.
2020: Cochrane review on laparoscopic surgery
A 2020 Cochrane systematic review found that for all types of endometriosis, "it is uncertain whether laparoscopic surgery improves overall pain compared to diagnostic laparoscopy".
2020: Stigma in Puerto Rico
A study done in Puerto Rico in 2020 found that health care and interactions with friends and family related to discussing endometriosis were affected by stigma.
2020: Recommendations for MRI for endometriosis
In 2020, an article recommended specific procedures for administering MRI for better image quality, including administering an anti-spasmodic agent, drinking a large glass of water, and scanning in the supine position with an abdominal strap.
2020: Classification of Endometriosis as a Syndrome
Reviews in 2020 concluded that endometriosis should be classified as a syndrome that requires confirmation of visible lesions seen at laparoscopy in addition to characteristic symptoms.
2021: Meta-analysis of treatments for endometriosis
A 2021 meta-analysis found that GnRH analogues and combined hormonal contraceptives were the best treatment for reducing dyspareunia, menstrual and non menstrual pelvic pain.
2025: Earnings and endometriosis diagnosis in the UK
A study published in the UK in 2025 found that after women received a diagnosis of endometriosis in an English NHS hospital their earnings were on average £56 per month less in the four to five years after diagnosis than they were in the two years before.
Mentioned in this timeline
Puerto Rico is a self-governing Caribbean archipelago and island that...
Trending

3 minutes ago Medvedev to clash with Auger-Aliassime in Dubai semifinals at Duty Free Tennis.

3 minutes ago Friday's Weather: Snow Returns After Brief Mildness, Lighter Winds Expected, End of Workweek.
4 minutes ago Lindsay Lohan reflects on troubled teen years and rebuilding her life in Dubai.
1 hour ago Ameren Prices $400M Senior Notes, $900M Bonds for Grid Investment, Reshaping Debt
2 hours ago Pokemon Celebrates 30 Years: A Cultural Phenomenon with Multimillion-Dollar Cards

2 hours ago Daylight Saving Time 2026: Prepare to set your clocks forward and lose sleep.
Popular

Jesse Jackson is an American civil rights activist politician and...

Barack Obama the th U S President - was the...

Susan Rice is an American diplomat and public official prominent...
XXXTentacion born Jahseh Dwayne Ricardo Onfroy was a controversial yet...

Michael Joseph Jackson the King of Pop was a highly...

Kashyap Pramod Patel is an American lawyer who became the...