Remdesivir, commercially known as Veklury, is a broad-spectrum antiviral drug created by Gilead Sciences. The drug is administered intravenously and gained widespread use during the COVID-19 pandemic. It received approval or emergency authorization for treating COVID-19 in many countries.
2009: Creation and development of remdesivir
In 2009, Gilead Sciences originally created and developed remdesivir to treat hepatitis C and respiratory syncytial virus (RSV). Despite not being effective against these viruses, it was repurposed for Ebola and Marburg virus research under scientist Tomáš Cihlář, showing antiviral activity against various viruses.
October 2015: USAMRIID announces preclinical results
In October 2015, USAMRIID announced that preclinical results showed remdesivir blocked the Ebola virus in Rhesus monkeys. This resulted from a collaboration between USAMRIID and Gilead Sciences, with initial screening performed by CDC scientists.
February 2016: European Commission Grants Orphan Designation to Remdesivir for Ebola Virus Disease
In February 2016, the European Commission granted orphan designation (EU/3/16/1615) to Gilead Sciences International Ltd for remdesivir as a treatment for Ebola virus disease.
2018: Mutations in Mouse Hepatitis Virus Lead to Partial Remdesivir Resistance
In 2018, researchers discovered mutations in the mouse hepatitis virus RNA replicase that caused partial resistance to remdesivir. These mutations hinder the virus's effectiveness in nature. Researchers believe these mutations are unlikely to persist where remdesivir is not being used.
April 2019: USPTO grants remdesivir patents
In April 2019, the USPTO granted two patents on remdesivir to Gilead Sciences: one for filoviruses and one covering both arenaviruses and coronaviruses.
August 2019: Efficacy in Ebola treatment
In August 2019, Congolese health officials announced that remdesivir was significantly less effective than monoclonal antibody treatments during the Kivu Ebola epidemic. However, the trials established its safety profile.
2019: GS-441524 Shows Promise in Treating Feline Infectious Peritonitis
In 2019, GS-441524, a metabolite of remdesivir, demonstrated potential in treating feline infectious peritonitis, a coronavirus-related illness in cats. However, it's crucial to note that the US FDA hadn't yet evaluated or approved it for this specific use. Despite this, GS-441524 became available through unregulated channels. The similarity in potency between GS-441524 and remdesivir against SARS-CoV-2 in lab settings led some researchers to propose directly administering GS-441524 as a COVID-19 treatment.
January 2020: Gilead Initiates Remdesivir Production Restart
Gilead began efforts to restart remdesivir production at its Edmonton, Alberta facility in January 2020.
January 2020: Gilead Ramps Up Remdesivir Production
In January 2020, Gilead Sciences began restarting and streamlining the complex production process for remdesivir. This involved sourcing 70 raw materials, reagents, and catalysts and optimizing a 25-step chemical synthesis. Notably, the production time was reduced from 9-12 months to 6 months to meet the rising demand for the drug.
February 2020: Gilead Ships Existing Remdesivir Stock
On February 2, 2020, Gilead transported its entire remaining stock of remdesivir, amounting to 100 kilograms in powder form, to its California filling plant to begin vial-filling procedures.
March 2020: Czech Republic Grants Provisional Approval for Remdesivir
Due to the escalating COVID-19 outbreak, the Czech Republic granted provisional approval for using remdesivir in treating severely ill COVID-19 patients in March 2020.
March 2020: Mexico Authorizes Remdesivir for Emergency Use
In March 2020, Cofepris granted emergency use authorization for remdesivir in Mexico, but advised continuous patient monitoring.
March 2020: US Approves Remdesivir for Compassionate Use
President Trump announced compassionate use access to remdesivir for COVID-19 patients in March 2020, later confirmed by the FDA.
April 2020: Limited Access to Remdesivir in Canada through Clinical Trials and Special Access Program
As of April 11, 2020, access to remdesivir in Canada was restricted to clinical trials. Health Canada granted approval for twelve individuals to receive remdesivir treatment under its Special Access Program (SAP), but further access was limited to pregnant women and children with confirmed and severe COVID-19.
April 2020: Gilead Estimates Remdesivir Production Capacity
By April 2020, Gilead estimated having enough remdesivir for 140,000 treatment courses, aiming to reach 500,000 by October and 1 million by year-end.
April 2020: First New Batch of Remdesivir Produced in Edmonton
By April 2020, the Edmonton plant had completed its first new batch of remdesivir. Concurrently, shipments of new raw materials from reactivated contract manufacturers began to arrive.
April 2020: EMA Issues Recommendations on Compassionate Use of Remdesivir for COVID-19 in the EU
The European Medicines Agency provided recommendations on the compassionate use of remdesivir for COVID-19 within the European Union in April 2020.
May 2020: Gilead Grants Remdesivir Licensing Agreements to Generic Drug Manufacturers
In May 2020, Gilead announced non-exclusive voluntary licensing agreements with five generic drug manufacturers in India and Pakistan. This enables the production and distribution of remdesivir in 127 countries. The agreements empower licensees to set their own prices and defer royalty payments to Gilead until the WHO declares the end of the COVID-19 emergency or the approval of another medicine or vaccine for COVID‑19.
May 2020: EMA Recommends Expanded Compassionate Use of Remdesivir for COVID-19
In May 2020, the EMA's Committee for Medicinal Products for Human Use (CHMP) recommended expanding the compassionate use of remdesivir for COVID-19 to include patients not on mechanical ventilation. This expanded use encompassed hospitalized individuals needing supplemental oxygen, non-invasive ventilation, high-flow oxygen devices, or ECMO. Additionally, a five-day treatment duration was introduced, alongside the existing ten-day course, based on preliminary study findings suggesting similar efficacy for patients not requiring mechanical ventilation or ECMO. Patients receiving the five-day treatment but not showing improvement were eligible to continue treatment for another five days.
May 2020: FDA Grants Emergency Use Authorization for Remdesivir
In May 2020, the FDA granted emergency use authorization for remdesivir in hospitalized adults and children with severe COVID-19.
May 2020: FDA Approves Remdesivir for COVID-19 Treatment, Revises EUA for Pediatric Use
In May 2020, the FDA granted its first approval for a COVID-19 treatment: remdesivir. However, the approval did not include the full patient population previously covered under the Emergency Use Authorization (EUA). To address this, the FDA revised the EUA to include hospitalized pediatric patients weighing 3.5 kilograms to less than 40 kilograms or those under twelve years of age weighing at least 3.5 kilograms.
May 2020: NIAID starts ACTT-2 trial
In May 2020, the National Institute of Allergy and Infectious Diseases (NIAID) started the Adaptive COVID-19 Treatment Trial 2 (ACTT-2) to evaluate the safety and efficacy of remdesivir plus baricitinib for treating hospitalized adults with confirmed SARS-CoV-2 infection and lung involvement.
May 2020: Japan Approves Remdesivir for COVID-19 Treatment
Japan's Ministry of Health, Labour and Welfare expedited the approval process for remdesivir, granting authorization for its use in treating COVID-19 in May 2020. This decision was based on the emergency authorization previously granted in the United States.
May 2020: US Remdesivir Distribution Faces Initial Challenges
The initial distribution of remdesivir in the US in May 2020 faced logistical challenges and confusion, leading to frustration among healthcare providers.
June 2020: Gilead Submits Application for Remdesivir Use in Canada
Gilead submitted an application to Health Canada in June 2020, seeking approval for the use of remdesivir in treating COVID-19.
June 2020: Gilead sets price for remdesivir
In June 2020, Gilead announced the pricing for remdesivir at US$390 per vial for governments of developed countries and US$520 for US private health insurance companies. The total cost for a treatment course of six vials over five days was set at US$2,340. The minimum production cost was estimated to be US$0.93 per day of treatment.
June 2020: Ligand Pharmaceuticals' Role in Remdesivir Delivery
In June 2020, Ligand Pharmaceuticals revealed its contribution to addressing the challenges of remdesivir's low solubility and stability. They achieved this by combining remdesivir with their proprietary excipient, Captisol, in a 30:1 ratio. To meet the increased demand for Captisol, Ligand is actively working on expanding its annual production capacity.
June 2020: HHS and Gilead Reach Agreement on Remdesivir Allocation
In June 2020, the US HHS agreed to purchase remdesivir from Gilead at wholesale price, allocating over 90% of the projected output for American patients until September 2020.
June 2020: India Grants Emergency Approval for Generic Remdesivir
On June 23, 2020, India granted emergency marketing approval for generic remdesivir produced by two of Gilead's licensees: Cipla and Hetero Drugs.
June 2020: Singapore Conditionally Approves Remdesivir
Singapore's Health Sciences Authority granted conditional approval for remdesivir use in June 2020.
July 2020: Australia Provisionally Approves Remdesivir for COVID-19 Treatment
In July 2020, Australia granted provisional approval for remdesivir's use in treating adults and adolescents with severe COVID-19 symptoms requiring hospitalization. The country stated it had procured a sufficient supply of remdesivir for its national stockpile.
July 2020: EU Grants Conditional Marketing Authorization for Remdesivir for COVID-19 Treatment
In July 2020, the European Union granted a conditional marketing authorization for remdesivir specifically for treating COVID-19 in adults and adolescents (aged twelve and above, weighing at least 40 kilograms) suffering from pneumonia and requiring supplemental oxygen.
July 2020: EU secures remdesivir contract
In July 2020, the European Union secured a €63 million contract with Gilead to make remdesivir available in early August 2020.
July 2020: Health Canada Conditionally Approves Remdesivir for COVID-19
On July 27, 2020, Health Canada granted conditional approval to Gilead's application for remdesivir use in treating COVID-19.
August 2020: FDA Expands EUA for Remdesivir to All Hospitalized COVID-19 Patients
In August 2020, the FDA broadened the EUA for remdesivir to include all hospitalized patients with suspected or confirmed COVID-19.
August 2020: NIAID starts ACTT 3 trial
In August 2020, the NIAID started the Adaptive COVID-19 Treatment Trial 3 (ACTT 3) to evaluate the safety and efficacy of a treatment regimen consisting of remdesivir plus interferon beta-1a for hospitalized adults with confirmed SARS-CoV-2 infection and lung involvement.
September 2020: Canada Secures Deal for Remdesivir Supply
Minister of Public Services and Procurement, Anita Anand, announced in September 2020 that Canada had secured an agreement with Gilead to receive up to 150,000 vials of remdesivir, with shipments commencing in October.
September 2020: HHS to Allocate Remdesivir to American Hospitals through September
The agreement between HHS and Gilead ensured the allocation of remdesivir to American hospitals would continue through September 2020.
October 2020: Gilead Projects Reaching 1 Million Remdesivir Treatment Courses
Gilead projected reaching a production capacity of one million remdesivir treatment courses by October 2020.
October 2020: Joint procurement framework contract signed
In October 2020, Gilead Sciences and the European Commission announced a joint procurement framework contract. Gilead agreed to provide up to 500,000 remdesivir treatment courses over six months to 37 European countries, including all 27 EU member states and other countries. The total contract value was approximately €1.035 billion.
October 2020: Mexico's Cofepris Rejects Remdesivir Approval
In October 2020, Mexico announced it would not approve remdesivir due to insufficient evidence of efficacy, as per Cofepris's assessment.
October 2020: FDA Approves Remdesivir for Hospitalized Adults and Children
In October 2020, the FDA approved remdesivir for adults and children (12 years and older) requiring hospitalization for severe COVID-19.
October 2020: FDA approval of remdesivir
In October 2020, the FDA approved remdesivir for medical use in the United States, based on data from three clinical trials involving 2043 hospitalized participants with COVID-19.
October 2020: FDA Approves Remdesivir and Expands EUA for Children
The FDA fully approved remdesivir and revised the EUA to include children weighing over 3.5 kg, a decision drawing criticism for lack of prior consultation.
October 2020: HHS Ends Control Over Remdesivir Allocation
With remdesivir production meeting US demand, HHS ended its control over allocation in October 2020, with AmerisourceBergen remaining the sole distributor.
November 2020: FDA Authorizes Baricitinib and Remdesivir Combination
In November 2020, the FDA issued an EUA for baricitinib in combination with remdesivir for hospitalized COVID-19 patients requiring supplemental oxygen or ventilation.
November 2020: FDA issues EUA for baricitinib with remdesivir
In November 2020, the FDA issued an emergency use authorization (EUA) for baricitinib, in combination with remdesivir, for treating hospitalized patients with COVID-19. The EUA was based on a randomized clinical trial conducted by the NIAID.
November 2020: FDA Authorizes Remdesivir Combination Therapy
In November 2020, the FDA issued an emergency use authorization for a combination therapy of baricitinib and remdesivir. This authorization allowed for the treatment of suspected or laboratory-confirmed COVID‑19 in hospitalized patients two years of age or older requiring supplemental oxygen, invasive mechanical ventilation, or ECMO.
November 2020: WHO updates remdesivir guidelines
In November 2020, the WHO updated its guideline to include a conditional recommendation against remdesivir for COVID-19, based on results from the WHO Solidarity trial.
January 2022: Study on remdesivir for nonhospitalized patients
In January 2022, a study indicated that nonhospitalized people at high risk for COVID-19 progression had an 87% lower risk of hospitalization or death after a 3-day course of intravenous remdesivir.
January 2022: Canadian Solidarity Trial report
In January 2022, the Canadian component of the WHO Solidarity Trial reported that in-hospital COVID-19 patients treated with remdesivir had a 17% lower relative risk of death and a 47% reduced relative risk for needing oxygen and mechanical ventilation.
January 2022: FDA Approves Remdesivir for Non-Hospitalized High-Risk Individuals
The FDA expanded remdesivir's approval in January 2022 to include non-hospitalized adults and children (12 years and older, weighing at least 40 kg) with COVID-19 and at high risk of severe illness.
April 2022: FDA Expands Remdesivir Approval to Include Younger Children
In April 2022, the FDA further expanded remdesivir's approval to include children as young as 28 days old weighing at least 3 kg.
August 2022: EU Grants Full Marketing Authorization for Remdesivir
The European Union granted full marketing authorization for remdesivir in August 2022, marking a significant milestone in the drug's regulatory journey.
September 2022: WHO updates remdesivir recommendation
In September 2022, the WHO updated guidelines to recommend remdesivir for both non-hospitalized and hospitalized patients, based on final results from the SOLIDARITY trial showing reduced mortality or progression to mechanical ventilation for non-ventilated patients.
2022: FDA Authorizes Remdesivir for Young Children with Mild-to-Moderate COVID-19
In 2022, the FDA granted emergency use authorization for remdesivir to treat children under 12 years old who are not hospitalized but have mild-to-moderate COVID-19 and are at high risk of severe illness.
Mentioned in this timeline
California is a U S state on the Pacific Coast...
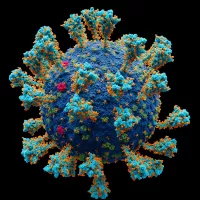
Coronaviruses are a family of RNA viruses affecting mammals and...
India officially the Republic of India is a South Asian...
Japan is an East Asian island country located in the...
Australia officially the Commonwealth of Australia encompasses the Australian mainland...
Canada is a North American country the second largest in...
Trending

32 minutes ago Oklahoma Sooners Honor Buddy Hield and 2016 Final Four Team.
32 minutes ago Moldova's Veterinary Education to modernize through the EDUVET European Project for enhancement.

32 minutes ago Brendan Fraser as Eisenhower in 'Pressure': D-Day drama unfolds with weather worries.

33 minutes ago Cade Cunningham's 42 Points Leads Pistons Over Knicks; Brunson's Performance Notable.

33 minutes ago Usha Vance's diaper request sparks controversy during pregnancy: A novel approach?

2 hours ago Learner Tien at Delray Beach Open: Fritz ousted, Paul advances, Korda previewed.
Popular

Jesse Jackson is an American civil rights activist politician and...

Barack Obama the th U S President - was the...

Bernie Sanders is a prominent American politician currently serving as...
Ken Paxton is an American politician and lawyer serving as...

Michael Joseph Jackson the King of Pop was a highly...
Randall Adam Fine is an American politician a Republican who...