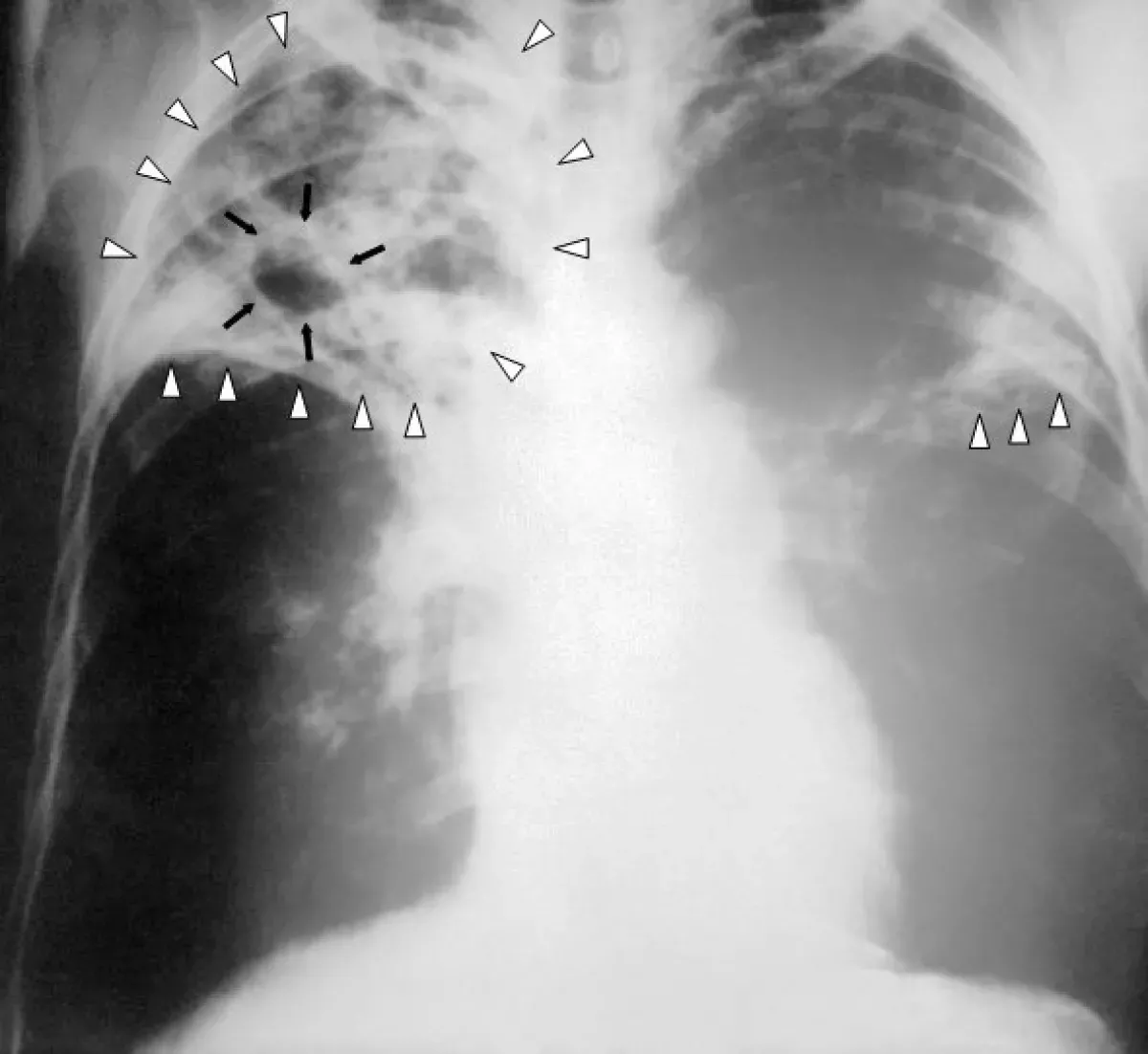
Tuberculosis (TB), historically known as consumption, is a contagious disease typically caused by Mycobacterium tuberculosis bacteria. It primarily affects the lungs but can impact other organs. Most infections are latent, showing no symptoms. However, about 10% of latent infections become active, potentially fatal if untreated. Active TB symptoms include chronic cough with bloody mucus, fever, night sweats, and weight loss. Infections in other organs can manifest diverse symptoms.
1905: Nobel Prize for Tuberculosis Discovery
Robert Koch received the Nobel Prize in Physiology or Medicine in 1905 for his discovery and description of the tuberculosis bacillus, Mycobacterium tuberculosis, in 1882.
1906: First Tuberculosis Immunization Success
Albert Calmette and Camille Guérin achieved the first real success in tuberculosis immunization using an attenuated bovine strain in 1906, which was later called the bacille Calmette-Guérin (BCG) vaccine.
1913: Focus on Tuberculosis Research
Upon its formation in 1913, the British Medical Research Council prioritized tuberculosis research.
1913: Medical Research Council and Tuberculosis Research
When the Medical Research Council was formed in Britain in 1913, its initial research focus was tuberculosis, highlighting the disease's continued threat to public health despite improvements.
1916: Sanatoria Treatment Outcomes
By around 1916, even with improved care in sanatoria, the mortality rate for tuberculosis patients remained high, with 50% dying within five years of admission.
1918: Tuberculosis Mortality in France
By 1918, tuberculosis was still a significant cause of death in France, accounting for one in six deaths.
1921: BCG Vaccine First Used on Humans
In 1921, the BCG vaccine was first administered to humans in France.
1945: Tuberculosis in Popular Culture
In 1945, tuberculosis continued to be a prominent theme across various forms of media, including literature (Thomas Mann's "The Magic Mountain"), music (Van Morrison's "T.B. Sheets"), opera (Puccini's "La bohème" and Verdi's "La Traviata"), art (Munch's painting of his sister), and film (The Bells of St. Mary's).
1946: Streptomycin Revolutionizes Tuberculosis Treatment
The development of streptomycin in 1946 marked a significant advancement in tuberculosis treatment, offering an effective cure and replacing previous surgical interventions.
1950: Decline in Tuberculosis Deaths in Europe
By 1950, deaths from tuberculosis in Europe had significantly decreased to 50 out of 100,000, compared to 500 out of 100,000 in 1850. This decline was attributed to improvements in public health.
1965: Tuberculosis Mortality Rate in Russia
In 1965, Russia's TB mortality rate was 61.9 per 100,000.
1990: China's progress against TB begins
In 1990, China embarked on significant efforts to control TB.
1993: Significant Decline in Russia's TB Mortality Rate
By 1993, Russia's TB mortality rate had dramatically dropped to 2.7 per 100,000.
1993: Tuberculosis Declared a Global Health Emergency
The rise of drug-resistant tuberculosis strains in the 1980s led to a resurgence of the disease, prompting the World Health Organization (WHO) to declare a global health emergency in 1993.
1995: New Respirator Regulations
In 1995, NIOSH implemented new respirator regulations, such as the N95, as part of the response to the spread of tuberculosis.
1995: Tuberculosis Mortality Rate
In 1995, the mortality rate for tuberculosis was around 8%.
1995: Start of WHO Tracking of Tuberculosis Cases
The WHO began its tracking of tuberculosis cases in 1995.
1997: Proposed Tuberculosis Rule by OSHA
In 1997, OSHA proposed new rules for tuberculosis, responding to pressure from advocacy groups like the Labor Coalition to Fight TB in the Workplace.
1998: Tuberculosis in Rural Canada
As of 1998, tuberculosis remained endemic in certain rural areas of Canada.
2000: India's TB Mortality Rate
India's estimated TB mortality rate in 2000 was 55 per 100,000 population.
2002: Decline in New Tuberculosis Cases
The number of new tuberculosis cases started declining in 2002.
2003: OSHA Withdraws Proposed Tuberculosis Rules
OSHA abandoned its proposed tuberculosis rules in 2003, due to declining tuberculosis cases in the US and public opposition.
2003: First Observation of Totally Drug-Resistant TB
Totally drug-resistant TB (TDR-TB), resistant to all known drugs, was first observed in 2003 in Italy.
2004: Decline in New TB Cases in China
Between 2004 and 2014, China witnessed a 17% decrease in new TB cases.
2005: Increase in Tuberculosis Mortality Rate in Russia
In 2005, the tuberculosis mortality rate in Russia increased to 24 per 100,000.
2005: Decline in Total Tuberculosis Cases
The total number of tuberculosis cases began decreasing in 2005.
2006: Research on New TB Vaccines
As of 2006, due to the limitations of the BCG vaccine, research into new TB vaccines was underway, with several candidates in clinical trials. Two main strategies were being pursued: adding a subunit vaccine to BCG and developing new live vaccines. One example is MVA85A, a subunit vaccine based on a modified vaccinia virus, being trialed in South Africa. Vaccines were expected to play a crucial role in treating both latent and active TB.
2006: Global Plan to Stop Tuberculosis
In 2006, the Stop TB Partnership launched the Global Plan to Stop Tuberculosis, aiming to save 14 million lives by 2015, although several targets were missed due to the rise of HIV-associated and drug-resistant tuberculosis.
2006: Incentivizing TB Vaccine Development
In 2006, to encourage further research, new economic models for vaccine development were being promoted, including prizes, tax breaks, and advance market commitments. Organizations such as the Stop TB Partnership, the South African Tuberculosis Vaccine Initiative, and the Aeras Global TB Vaccine Foundation (which received over US$280 million from the Gates Foundation) were actively involved.
2007: Rifabutin Use in HIV-Positive Individuals with Tuberculosis
As of 2007, the benefit of routinely using rifabutin instead of rifampicin for HIV-positive individuals with tuberculosis was unclear.
2007: Eswatini with Highest TB Incidence Rate
In 2007, Eswatini had the world's highest estimated TB incidence rate, at 1,200 cases per 100,000 people.
2008: Tuberculosis Mortality Rate Decreases
By 2008, the mortality rate for tuberculosis had decreased to about 4%, compared to 8% in 1995.
2009: Economic Burden and Challenges in TB Eradication
In 2009, the World Bank estimated the annual cost of TB in high-burden countries to exceed US$150 billion. Lack of patient follow-up, such as among rural migrants in China, also hindered eradication efforts. While universal TB care in countries like Brazil showed promise, the decline in TB rates may also be linked to broader improvements in education, income, and overall health.
2010: Recommended Tuberculosis Treatment in 2010
As of 2010, the standard treatment for new pulmonary tuberculosis cases involved a six-month antibiotic regimen. This regimen consisted of rifampicin, isoniazid, pyrazinamide, and ethambutol for the initial two months, followed by rifampicin and isoniazid for the remaining four months. In cases of high isoniazid resistance, ethambutol could be added for the last four months. While shorter treatments were considered for compliance issues, there wasn't strong evidence supporting their efficacy compared to the six-month regimen.
2010: China's Success in Reducing TB Mortality
By 2010, China had achieved an 80% reduction in its TB mortality rate compared to 1990.
2010: India's TB Burden
In 2010, India had the world's highest number of TB cases, partly due to challenges in disease management within both private and public healthcare sectors. Initiatives like the Revised National Tuberculosis Control Program are working to address this issue within the public health system.
2010: Tuberculosis Rates per 100,000 People
In 2010, global tuberculosis rates were reported as 178 per 100,000 people. Regional rates varied, with Africa at 332, the Americas at 36, Eastern Mediterranean at 173, Europe at 63, Southeast Asia at 278, and Western Pacific at 139.
2010: Addressing TB Stigma
In 2010, strategies to reduce TB stigma included promoting "TB clubs" for support and sharing experiences, and implementing educational programs. However, research on the link between reduced stigma and mortality was lacking, and similar efforts for AIDS had limited success. Stigma was sometimes considered worse than the disease itself, and healthcare providers could unintentionally reinforce it. A greater understanding of the social and cultural aspects of TB was seen as crucial for stigma reduction.
2010: New Tuberculosis Diagnoses and Deaths
In 2010, there were approximately 8.8 million new tuberculosis diagnoses and between 1.20 and 1.45 million deaths, mostly in developing nations. Of these deaths, about 0.35 million were in individuals co-infected with HIV.
2011: Limited TB Diagnostic Access
As of 2011, many resource-poor regions had limited access to TB diagnostics, relying primarily on sputum microscopy.
2012: New Medication Regimen for Multidrug-Resistant TB
A new medication regimen for multidrug-resistant tuberculosis was approved in the US in 2012, featuring bedaquiline alongside existing drugs. Initial safety concerns were later allayed by larger studies, and by 2017, the regimen was used in at least 89 countries.
2012: Subsidized TB Testing
In 2012, the WHO, Gates Foundation, and US government began subsidizing a fast-acting diagnostic test for TB in low- and middle-income countries. This test can also detect rifampicin resistance, which can indicate multi-drug resistant TB, and is accurate even in patients with HIV.
2012: Estimated Active Tuberculosis Cases
In 2012, there were an estimated 8.6 million active cases of tuberculosis chronically.
2013: Delamanid Approval for Multidrug-Resistant TB
Delamanid was approved by the European Medicines Agency in 2013 for multidrug-resistant tuberculosis.
2014: Call for Increased TB Funding
A 2014 EIU-healthcare report highlighted the need to address apathy and increase funding for TB, noting its neglect even in high-burden countries and by donors.
2014: Continued Progress in Reducing New TB Cases in China
By 2014, China had further decreased its incidence of new TB cases compared to 2004.
2014: Push for Transparency and Regulation in TB Treatment
In 2014, international organizations advocated for more transparency in TB treatment, with more countries implementing mandatory case reporting. However, adherence varied, and concerns arose about overprescription of second-line drugs and supplementary treatments by commercial providers.
2014: WHO's "End TB" Strategy
In 2014, the WHO launched the "End TB" strategy, aiming to reduce TB incidence by 80% and mortality by 90% by 2030, with interim goals for 2020.
2015: Decline in India's TB Mortality Rate and Estimated Deaths
By 2015, India's estimated TB mortality rate had decreased to 36 per 100,000 population, with an estimated 480,000 deaths.
2015: Decrease in Tuberculosis Mortality Rate in Russia
By 2015, the tuberculosis mortality rate in Russia decreased to 11 per 100,000.
2015: TB Deaths and Incidence in South Africa
In 2015, the TB incidence rate in South Africa was 988 per 100,000, with a total of 552,000 cases.
2015: Tuberculosis in Captive Elephants
In 2015, tuberculosis was found to be widespread among captive elephants in the US, believed to be transmitted from humans (reverse zoonosis). This posed a public health risk in circuses and zoos due to airborne transmission.
2015: End TB Strategy
The End TB Strategy, launched in 2015, aims to reduce tuberculosis deaths by 95% and incidence by 90% by 2035.
2017: Global Use of Bedaquiline and Delamanid
By 2017, bedaquiline was used in at least 89 countries and delamanid in at least 54 for multidrug-resistant tuberculosis.
2017: Lesotho with Highest Estimated TB Incidence Rate
In 2017, Lesotho had the highest estimated TB incidence rate, with 665 cases per 100,000 people.
2017: Tuberculosis Incidence in the UK and Western Europe
In 2017, the UK's national average TB incidence was 9 per 100,000. Portugal had the highest rate in Western Europe at 20 per 100,000.
2017: India's High TB Incidence
India had the highest total TB incidence in 2017, with an estimated 2,740,000 cases.
2018: Global Tuberculosis Statistics
In 2018, a quarter of the world's population was estimated to have latent TB, with new infections occurring in 1% of the population annually. Most cases were in South-East Asia, Africa, and the Western Pacific, with India, China, Indonesia, the Philippines, Pakistan, Nigeria, and Bangladesh accounting for over 50% of diagnoses.
2018: Tuberculosis as Leading Cause of Death
In 2018, tuberculosis was the leading cause of death worldwide from a single infectious agent.
2019: Changes in Tuberculosis Testing Recommendations
In 2019, the Centers for Disease Control and Prevention (CDC) stopped recommending annual tuberculosis testing for healthcare workers without known exposure.
2020: "End TB" Strategy Milestone Year
By 2020, the WHO's "End TB" strategy aimed to achieve interim milestones of a 20% reduction in TB incidence and a 35% reduction in deaths. However, these targets were missed globally, although some regions made better progress. Treatment, prevention, and funding milestones were also not met.
2020: New Four-Month Tuberculosis Treatment Regimen
In 2020, a clinical trial presented findings on a new four-month treatment regimen for drug-susceptible tuberculosis. This regimen involves a high-dose rifapentine combined with moxifloxacin (2PHZM/2PHM). The results indicated that this shorter regimen is as safe and effective as the standard six-month treatment.
2021: BCG Vaccine Efficacy
As of 2021, the BCG vaccine remained the only available tuberculosis vaccine. In children, it reduces the risk of infection by 20% and the risk of progression to active disease by almost 60%.
2021: Tuberculosis Incidence
By 2021, the number of new tuberculosis cases annually was declining by about 2%.
2021: Tuberculosis Case Rate in Canada
In 2021, the overall tuberculosis case rate in Canada was 4.8 per 100,000 persons. The rates were significantly higher among Inuit (135.1 per 100,000), First Nations (16.1 per 100,000), and people born outside Canada (12.3 per 100,000).
2022: TB Deaths and Incidence in South Africa
In 2022, 54,200 people died from TB in South Africa. The incidence rate was 468 per 100,000, with a total of 280,000 cases.
2022: Tuberculosis Mortality
In 2022, active TB developed in an estimated 10.6 million people, resulting in 1.3 million deaths, making it the second leading cause of death from an infectious disease after COVID-19.
2022: Tuberculosis Cases and Deaths in 2022
In 2022, there were 7.5 million new cases of TB diagnosed, and 1.32 million deaths attributed to the disease.
2022: Tuberculosis Case Rate in the United States
The tuberculosis case rate in the United States in 2022 was 2.5 per 100,000, which was lower compared to the 2.9 per 100,000 rate in 2023.
2023: Tuberculosis Case Rate and Disparities in the United States
In 2023, the tuberculosis case rate in the U.S. was 2.9 per 100,000, a 16% increase from 2022. Racial and ethnic minorities represented 88% of reported cases, with Native Americans experiencing a fivefold higher mortality rate.
2023: Tuberculosis Overtakes COVID-19 as Leading Cause of Infectious Disease Deaths
In 2023, tuberculosis surpassed COVID-19 as the leading cause of infectious disease-related deaths globally. Around 8.2 million new cases were diagnosed, a record high since WHO tracking began in 1995. Deaths decreased to 1.25 million from 1.32 million in 2022, while the overall cases rose to 10.8 million.
2030: Target Year for "End TB" Strategy
2030 is the target year set by the WHO's "End TB" strategy to achieve an 80% reduction in TB incidence and a 90% reduction in deaths.
Mentioned in this timeline
Nigeria is a West African nation the most populous in...
India officially the Republic of India is a South Asian...
China officially the People's Republic of China is an East...
Africa is the second-largest and second-most populous continent comprising of...

The World Bank is an international financial institution offering loans...

The World Health Organization WHO is a specialized agency of...
Trending

1 minute ago CDC Panel to Discuss COVID-19 Vaccine Injuries Following RFK Jr.'s Meeting

2 minutes ago Casey Means' Surgeon General Nomination Faces Scrutiny Over Mainstream Medicine Criticism and Birth Control Views.
1 hour ago Punch, the lonely baby monkey, goes viral and wins hearts worldwide.
2 hours ago Jon Hamm Discovers Viral Dancing Meme; Reacts to Meme-Worthy Status at 54.
2 hours ago Georgia: Missing child found safe after Amber Alert issued in Barrow County.

3 hours ago Selena Gomez Defends Benny Blanco Amid Dirty Feet Frenzy and Divorce Comments.
Popular

Jesse Jackson is an American civil rights activist politician and...

Barack Obama the th U S President - was the...

Susan Rice is an American diplomat and public official prominent...
XXXTentacion born Jahseh Dwayne Ricardo Onfroy was a controversial yet...

Michael Joseph Jackson the King of Pop was a highly...

Kashyap Pramod Patel is an American lawyer who became the...