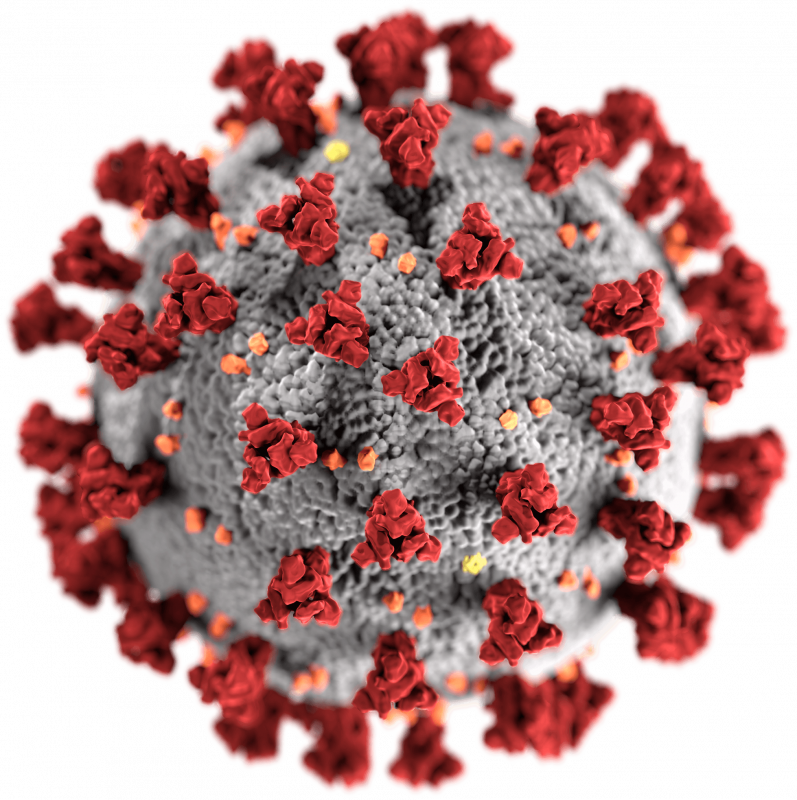
COVID-19 vaccines are designed to provide immunity against SARS-CoV-2, the virus causing COVID-19. Various types were developed rapidly, including mRNA, viral vector, and inactivated virus vaccines. They work by stimulating the body's immune system to recognize and fight the virus. Widespread vaccination has significantly reduced severe illness, hospitalization, and death rates. However, vaccine effectiveness can wane over time, and booster shots are recommended to maintain protection, especially against emerging variants. While generally safe, side effects can occur, typically mild and temporary. The vaccines remain a crucial tool in controlling the pandemic and mitigating its impact.
2003: Vaccines produced against animal coronaviruses
As of 2003, vaccines have been produced against several animal diseases caused by coronaviruses, including infectious bronchitis virus in birds, canine coronavirus, and feline coronavirus.
2005: SARS vaccine and medicine development prioritized
According to studies published in 2005, the identification and development of novel vaccines and medicines to treat SARS was a priority for governments and public health agencies around the world at that time.
2006: SARS vaccine and medicine development prioritized
According to studies published in 2006, the identification and development of novel vaccines and medicines to treat SARS was a priority for governments and public health agencies around the world at that time.
2015: Moderna begins human testing of an mRNA vaccine
In 2015, Moderna began human testing of an mRNA vaccine.
2019: SARS-CoV-2 isolated
In late 2019, SARS-CoV-2, the virus responsible for COVID-19, was isolated.
January 2020: Chinese vaccine developers begin efforts
In January 2020, Chinese vaccine developers and the Chinese Center for Disease Control and Prevention began their efforts, and by March they were pursuing numerous candidates on short timelines.
January 2020: Genetic sequence published
In January 2020, the genetic sequence of SARS-CoV-2, the virus causing COVID-19, was published, which initiated an urgent international response focused on outbreak preparation and accelerating COVID-19 vaccine development.
January 2020: Expedited vaccine development begins through collaboration
Since January 2020, COVID-19 vaccine development has been expedited via unprecedented collaboration in the multinational pharmaceutical industry and between governments.
February 2020: WHO anticipates vaccine availability in 18 months
In February 2020, the World Health Organization (WHO) estimated that a vaccine against SARS-CoV-2 would not be available for at least 18 months.
February 2020: US liability shields take effect
On February 4, 2020, US Secretary of Health and Human Services, Alex Azar, published a notice of declaration under the Public Readiness and Emergency Preparedness Act (PREP Act) for medical countermeasures against COVID‑19, which precluded liability claims alleging negligence by a manufacturer in creating a vaccine.
March 2020: MERS vaccine completes Phase I clinical trials
As of March 2020, there was one (DNA-based) MERS vaccine that completed Phase I clinical trials in humans, and three others in progress, all being viral-vectored vaccines: two adenoviral-vectored (ChAdOx1-MERS, BVRS-GamVac) and one MVA-vectored (MVA-MERS-S).
April 2020: Access to COVID‑19 Tools Accelerator announced
In April 2020, the Access to COVID‑19 Tools Accelerator, a G20 and World Health Organization (WHO) initiative, was announced to enable partners to share resources and knowledge.
April 2020: UK Agrees to Vaccine Collaboration and Sharing of Results
In April 2020, the UK agreed to collaborate with 20 other countries and global organizations to develop a COVID-19 vaccine, with a commitment to share the results. UK citizens would not receive preferential access to any new COVID‑19 vaccines developed by taxpayer-funded UK universities.
April 2020: UK government forms COVID‑19 vaccine task force
In April 2020, the United Kingdom government formed a COVID‑19 vaccine task force to stimulate local efforts for accelerated development of a vaccine through collaborations between industries, universities, and government agencies.
May 2020: US government announces funding for Operation Warp Speed
In May 2020, the US government announced funding for a fast-track program called Operation Warp Speed to support American COVID‑19 vaccine development.
June 2020: Billions of dollars invested in vaccine development
By June 2020, corporations, governments, international health organizations, and university research groups invested tens of billions of dollars to develop numerous vaccine candidates and prepare for global vaccination programs against COVID-19 infection.
June 2020: China Approves CanSino Vaccine for Limited Use
On 24 June 2020, China approved the CanSino vaccine for limited use in the military and also approved two inactivated virus vaccines for emergency use in high-risk occupations.
August 2020: Russia Approves Sputnik V Vaccine for Emergency Use
On 11 August 2020, Russia announced the approval of its Sputnik V vaccine for emergency use, although its distribution remained limited outside of the Phase 3 trial for a month.
September 2020: Eleven vaccine candidates use adjuvants to enhance immunogenicity
As of September 2020, eleven of the vaccine candidates in clinical development use adjuvants to enhance immunogenicity.
October 2020: TRIPS waiver proposed
The TRIPS waiver, which intended to temporarily waive intellectual property protections for COVID-19 vaccines, was first proposed in October 2020, gaining support from most countries but facing delays due to opposition from the EU, the UK, Norway, and Switzerland.
November 2020: High-Income Nations Purchase Majority of Pre-Sold Vaccine Doses
As of 15 November 2020, high-income nations, representing only 14% of the global population, had contracted to buy 51% of all pre-sold doses of COVID‑19 vaccines.
November 2020: Pfizer–BioNTech Submits EUA Request to FDA
On 20 November 2020, the Pfizer–BioNTech partnership submitted an Emergency Use Authorization (EUA) request to the U.S. Food and Drug Administration (FDA) for the mRNA vaccine BNT162b2.
December 2020: More than 10 billion COVID-19 vaccine doses preordered
By December 2020, more than 10 billion COVID-19 vaccine doses had been preordered by countries, with about half of the doses purchased by high-income countries comprising 14% of the world's population.
December 2020: Severe allergic reactions reported after Pfizer–BioNTech COVID‑19 vaccine administration
In December 2020, 1,893,360 first doses of Pfizer–BioNTech COVID‑19 vaccine administration resulted in 175 cases of severe allergic reactions, of which 21 were anaphylaxis.
December 2020: UK grants Pfizer legal indemnity
In December 2020, the UK government granted Pfizer legal indemnity for its COVID‑19 vaccine, providing legal protection against potential liabilities.
December 2020: UK Approves Pfizer-BioNTech Vaccine; Other Countries Follow
On 2 December 2020, the United Kingdom's Medicines and Healthcare products Regulatory Agency (MHRA) provided temporary regulatory approval for the Pfizer–BioNTech vaccine, becoming the first country to approve the vaccine. On 11 December 2020, the FDA granted an EUA for the Pfizer–BioNTech COVID‑19 vaccine and later granted an EUA for mRNA-1273, the Moderna vaccine. As of 21 December 2020, many countries and the European Union had authorized or approved the Pfizer–BioNTech COVID‑19 vaccine. Bahrain and the United Arab Emirates granted emergency marketing authorization for the Sinopharm BIBP vaccine.
December 2020: Start of COVID-19 Vaccine Rollout
The study that ran until December 2021, estimated that COVID-19 vaccines prevented an additional 14.4 to 19.8 million deaths in 185 countries and territories from 8 December 2020 to 8 December 2021.
2020: Distribution Considerations During COVID-19 Pandemic
During the rapid COVID-19 pandemic in 2020, international organizations, vaccine developers, governments, and industry evaluated the distribution of the eventual COVID-19 vaccine(s). Experts emphasized equitable access for healthcare frontlines and those in most need.
2020: First COVID‑19 vaccines developed and made available
In 2020, the first COVID‑19 vaccines were developed and made available to the public through emergency authorizations and conditional approvals.
2020: COVID-19 vaccine platforms developed
In 2020, various COVID-19 vaccine platforms were developed, including nucleic acid technologies (nucleoside-modified messenger RNA and DNA), non-replicating viral vectors, peptides, recombinant proteins, live attenuated viruses, and inactivated viruses.
January 2021: Anaphylaxis cases reported after Moderna COVID‑19 vaccine administration
For 4,041,396 Moderna COVID‑19 vaccine dose administrations in January 2021, only ten cases of anaphylaxis were reported.
January 2021: WHO Director-General Warns of Inequitable Vaccine Distribution
In January 2021, WHO Director-General Tedros Adhanom Ghebreyesus highlighted the issue of inequitable vaccine distribution, noting that while over 39 million doses had been administered in higher-income countries, only 25 doses had been given in one lowest-income country.
March 2021: BARDA funds COVID-19 vaccine development
By March 2021, the Biomedical Advanced Research and Development Authority (BARDA) had funded an estimated $19.3 billion in COVID‑19 vaccine development.
March 2021: Vaccination disparity in Brazil
In March 2021, Brazilian journalism agency Agência Pública reported that twice as many white individuals were vaccinated compared to Black individuals, while COVID-19 mortality rates were higher among the Black population, revealing racial disparities in vaccine access within Brazil.
March 2021: Covaxx raises $1.35 billion in private placement
In March 2021, Covaxx, a company associated with Erik Prince, raised $1.35 billion in a private placement to fund the development of its COVID-19 vaccine, UB-612.
March 2021: US Attempt to Influence Brazil's Vaccine Purchase; Access Blocked by Competing Nations
In March 2021, the US attempted to dissuade Brazil from purchasing the Sputnik V COVID‑19 vaccine due to concerns about "Russian influence". Access to vaccines was also reportedly blocked by competing nations in areas with territorial disputes, such as Palestine accusing Israel of blocking vaccine delivery and Taiwan suggesting that China has hampered its efforts to procure vaccine doses.
March 2021: Developed Countries Block COVID-19 Vaccine Patent Waiver
In March 2021, the United States, Britain, European Union member states, and some other members of the World Trade Organization (WTO) blocked a push by more than eighty developing countries to waive COVID‑19 vaccine patent rights.
March 2021: Russia Registers First COVID-19 Vaccine for Animals
On 31 March 2021, the Russian government announced the registration of Carnivac-Cov, the first COVID-19 vaccine for animals. It is an inactivated vaccine designed for carnivorous animals, including pets, to prevent SARS-CoV-2 mutations during interspecies transmission.
April 2021: WHO emergency committee addresses vaccine inequity
In April 2021, the World Health Organization's emergency committee addressed concerns of persistent inequity in global vaccine distribution.
May 2021: Global vaccine distribution inequity
As of May 2021, the World Health Organization reported that the 29 poorest countries, despite comprising 9% of the global population, had only received 0.3% of administered vaccines, highlighting the stark inequity in global vaccine distribution.
May 2021: UNICEF appeals for vaccine donations
In May 2021, UNICEF urgently appealed to industrialized nations to donate excess COVID-19 vaccine capacity to cover a 125-million-dose gap in the COVAX program.
May 2021: US Supports Waiving Intellectual Property Protections for COVID-19 Vaccines
On 5 May 2021, the US government under President Joe Biden announced its support for waiving intellectual property protections for COVID‑19 vaccines, with the European Parliament backing a motion to temporarily lift these rights.
June 2021: COVAX supply problems due to Indian domestic needs
From March to June 2021, the Serum Institute of India, a major supplier to the COVAX program with the Oxford–AstraZeneca COVID‑19 vaccine, faced supply problems because of increased domestic vaccine needs in India, impacting the availability of vaccines for the program.
June 2021: Erik Prince's involvement with Covaxx
In June 2021, a report revealed that the UB-612 vaccine, developed by Covaxx, was a for-profit venture initiated by Blackwater founder Erik Prince, who discussed the profit-making potential of selling COVID‑19 vaccines.
July 2021: Multiple technology platforms under research for COVID-19 vaccine
As of July 2021, at least nine different technology platforms were under research and development to create an effective vaccine against COVID‑19, focusing on the coronavirus spike protein (S protein) and its variants.
July 2021: Vaccine dose wastage reported
In July 2021, The BMJ reported that countries had discarded over 250,000 vaccine doses due to supply exceeding demand and strict laws preventing vaccine sharing. Additionally, The New York Times reported that over a million doses were wasted in ten U.S. states due to federal regulations and expiration dates.
July 2021: India to release CoWIN platform and Aarogya Setu source code
In July 2021, the Prime Minister of India, Narendra Modi, announced that India would make its digital vaccination management platform, CoWIN, open to the global community and release the source code for the contact tracing app Aarogya Setu for developers worldwide, with around 142 countries expressing interest.
July 2021: Joint statement on vaccine access
In July 2021, the heads of the World Bank Group, the International Monetary Fund, the World Health Organization, and the World Trade Organization issued a joint statement expressing deep concern about the limited availability of vaccines, therapeutics, diagnostics, and support for deliveries to developing countries.
August 2021: Delta Variant Dominance and Increased Risk for Unvaccinated
By late August 2021, the Delta variant accounted for 99 percent of U.S. cases and was found to double the risk of severe illness and hospitalization for those not yet vaccinated. The CDC also reported that vaccine effectiveness fell from 91% against Alpha to 66% against Delta.
August 2021: US announces plans for booster doses
In August 2021, the United States government announced plans to offer booster doses eight months after the initial course to the general population, starting with priority groups, despite criticism from the WHO.
August 2021: WHO calls for moratorium on booster doses
In August 2021, the WHO called for a moratorium on booster doses at least until the end of September to reduce unequal distribution between rich and poor countries.
August 2021: Sputnik V developers propose Pfizer test Ad26 component as booster
In August 2021, the developers of Sputnik V proposed, in view of the Delta case surge, that Pfizer test the Ad26 component (termed its 'Light' version) as a booster shot.
September 2021: Vaccine inequity damages global economy
As of September 2021, vaccine inequity damages the global economy, disrupting the global supply chain, and can cause rich countries to lose more money than poor ones, though the poor ones will lose a higher percentage of GDP and experience longer-term effects.
September 2021: Former world leaders call for waiving IP rules for COVID-19 vaccines
In September 2021, more than 140 former world leaders and Nobel laureates called on the candidates to be the next German chancellor to declare themselves in favor of waiving intellectual property rules for COVID‑19 vaccines and transferring vaccine technologies.
September 2021: Day of Action to pressure WTO on TRIPS waiver
Médecins Sans Frontières (Doctors without Borders) called for a Day of Action in September 2021 to put pressure on the WTO Ministerial meeting in November, which was expected to discuss the TRIPS IP waiver.
September 2021: Peru proposes international treaty for vaccine access
On September 21, 2021, during his first international trip, the President of Peru, Pedro Castillo, proposed the creation of an international treaty signed by world leaders and pharmaceutical companies to guarantee universal vaccine access at the seventy-sixth session of the United Nations General Assembly.
October 2021: Razi Cov Pars authorized as first intranasal vaccine in Iran
In October 2021, the first authorised intranasal vaccine was Razi Cov Pars in Iran.
November 2021: ECDC estimates lives saved by vaccination
In November 2021, a study by the ECDC estimated that 470,000 lives over the age of 60 had been saved since the start of the vaccination roll-out in the European region.
November 2021: Nursing unions appeal to UN over COVID-19 vaccine patents
In November 2021, nursing unions in 28 countries filed a formal appeal with the United Nations over the refusal of the UK, EU, Norway, Switzerland, and Singapore to temporarily waive patents for COVID‑19 vaccines.
November 2021: Full Nucleotide Sequences of Vaccines Released
In November 2021, the full nucleotide sequences of the AstraZeneca and Pfizer/BioNTech vaccines were released by the UK Medicines and Healthcare products Regulatory Agency in response to a freedom of information request.
December 2021: Study estimates millions of deaths prevented by vaccines
According to a June 2022 study, COVID‑19 vaccines prevented an additional 14.4 to 19.8 million deaths in 185 countries and territories from 8 December 2020 to 8 December 2021.
December 2021: CDC Data on Mortality Rates by Vaccination Status
According to early December 2021 CDC data, "unvaccinated adults were about 97 times more likely to die from COVID-19 than fully vaccinated people who had received boosters".
December 2021: Lack of Reliable Tests to Determine Protection from Infection
As of December 2021, there are no FDA-authorized or approved tests available for providers or the public to reliably determine if a person is protected from COVID-19 infection.
December 2021: UK Health Security Agency Reports Reduced Neutralizing Activity for Omicron
On 10 December 2021, the UK Health Security Agency reported that early data indicated a 20- to 40-fold reduction in neutralizing activity for Omicron by sera from Pfizer 2-dose vaccinees relative to earlier strains. After a booster dose, vaccine effectiveness against symptomatic disease was at 70%–75%, and the effectiveness against severe disease was expected to be higher.
2021: Low Risk of Subsequent Infection After Vaccination or Previous Infection
As of 2021, available evidence indicates that fully vaccinated individuals and those previously infected with SARS-CoV-2 have a low risk of subsequent infection for at least six months. However, there is insufficient data to determine a definitive antibody titer threshold for protection.
2021: CDC reports on vaccine effectiveness
In 2021, the CDC reported that unvaccinated people were 10 times more likely to be hospitalized and 11 times more likely to die than fully vaccinated people.
March 2022: Protection Decline in Elderly Care Home Residents
As of March 2022, protection against severe illness, hospitalization, and death among elderly residents in English care homes was high immediately after vaccination but declined significantly in the months following vaccination. Regular boosters are recommended for older people.
March 2022: Vaccine inequity persists
As of March 2022, the World Health Organization's goal of vaccinating 70% of the global population by mid-2022 was far from being achieved, with only one percent of the 10 billion doses given worldwide having been administered in low-income countries.
March 2022: White House releases "National COVID‑19 Preparedness Plan"
In March 2022, the White House released the "National COVID‑19 Preparedness Plan", which recommended accelerating the development of a universal coronavirus vaccine.
March 2022: CDC Recommends Fourth Dose of Pfizer mRNA Vaccine for Immunocompromised and Over 50s
As of March 2022, the US Centers for Disease Control and Prevention (CDC) recommends a fourth dose of the Pfizer mRNA vaccine for "certain immunocompromised individuals and people over the age of 50".
April 2022: Sputnik Nasal authorized in Russia
In April 2022, the first viral component of Sputnik V vaccine was authorised in Russia as Sputnik Nasal.
April 2022: SpFN vaccine begins Phase I clinical trial
In April 2022, the spike ferritin-based nanoparticle (SpFN) vaccine being developed at the Walter Reed Army Institute of Research, began a Phase I clinical trial.
May 2022: FDA limits the use of the Janssen Vaccine to very specific cases
On 5 May 2022 the FDA posted a bulletin limiting the use of the Janssen Vaccine to very specific cases due to further reassessment of the risks of TTS, although the FDA also stated in the same bulletin that the benefits of the vaccine outweigh the risks.
June 2022: Study estimates millions of deaths prevented by vaccines
According to a June 2022 study, COVID‑19 vaccines prevented an additional 14.4 to 19.8 million deaths in 185 countries and territories from 8 December 2020 to 8 December 2021.
June 2022: Pfizer and Moderna Develop Bivalent Vaccines
In June 2022, Pfizer and Moderna developed bivalent vaccines to protect against the SARS-CoV-2 wild-type and the Omicron variant. These vaccines offer immunity to Omicron superior to previous mRNA vaccines and are well-tolerated.
September 2022: Vaccination Rates in Low-Income Countries
By September 2022, only 22.3 percent of people in low-income countries had received at least a first COVID-19 vaccine dose.
September 2022: FDA Authorizes Bivalent Vaccines
In September 2022, the United States Food and Drug Administration (FDA) authorized the bivalent vaccines developed by Pfizer and Moderna.
September 2022: EU conditional marketing authorizations changed to standard authorizations
In the European Union, the COVID‑19 vaccines conditional marketing authorizations were changed to standard authorizations in September 2022. These authorizations do not exempt manufacturers from civil and administrative liability claims, even for side effects not known at the time of licensure.
October 2022: China Administers Oral Vaccine Developed by CanSino Biologics
In October 2022, China began administering an oral vaccine developed by CanSino Biologics, utilizing its adenovirus model.
November 2022: 40 vaccines authorized for public use
As of November 2022, 40 vaccines are authorized by at least one national regulatory authority for public use.
December 2022: China approves second intranasal vaccine as booster
In December 2022, China approved a second intranasal vaccine as a booster, trade name Pneucolin.
December 2022: Florida to investigate COVID-19 vaccines
On December 13, 2022, the governor of Florida, Ron DeSantis, announced his intention to petition the state supreme court to convene a grand jury to investigate potential violations related to COVID‑19 vaccines.
2022: Viral Load and Transmission with Delta Variant Breakthrough Infections
As of 2022, fully vaccinated individuals with breakthrough infections with the SARS-CoV-2 delta (B.1.617.2) variant were found to have a peak viral load similar to unvaccinated cases and could transmit infection in household settings.
2022: Delayed delivery of Moderna and Pfizer vaccines
In mid-May 2021, UNICEF criticized that most proposed donations of Moderna and Pfizer vaccines were not expected to be delivered until the second half of 2021 or early in 2022.
February 2023: Infection Protection Compared to Vaccination
In February 2023, a systematic review in The Lancet stated that the protection from infection was comparable to that from vaccination, but with a higher risk of severe illness and death from the initial infection.
March 2023: Bimervax approved for use as a booster vaccine in the European Union
In March 2023, Bimervax (selvacovatein) was approved for use as a booster vaccine in the European Union.
June 2023: FDA Advises Update to Monovalent COVID-19 Vaccine
In June 2023, the FDA advised manufacturers that the 2023–2024 formulation of the COVID‑19 vaccines for use in the US be updated to be a monovalent COVID‑19 vaccine using the XBB.1.5 lineage of the Omicron variant.
November 2023: Texas sues Pfizer over COVID-19 vaccine claims
In November 2023, the US state of Texas sued Pfizer under section 17.47 of the Texas Deceptive Trade Practices Act, alleging that the company misled the public about its COVID-19 vaccine by hiding risks while making false claims about its effectiveness.
2023: Nobel Prize awarded for mRNA COVID‑19 vaccines
In 2023, the Nobel Prize in Physiology or Medicine was awarded to Katalin Karikó and Drew Weissman for the development of effective mRNA vaccines against COVID‑19.
May 2024: Results of SpFN Phase I clinical trial published
In May 2024, the results of the Phase I clinical trial for the spike ferritin-based nanoparticle (SpFN) vaccine, developed at the Walter Reed Army Institute of Research, were published.
June 2024: FDA Advises Update to Monovalent COVID-19 Vaccine
In June 2024, the FDA advised manufacturers that the 2024–2025 formulation of the COVID‑19 vaccines for use in the US be updated to be a monovalent COVID‑19 vaccine using the JN.1 lineage.
June 2024: FDA advises COVID-19 vaccines for Fall 2024 should be monovalent JN.1 vaccines
In June 2024, the US Food and Drug Administration advised the manufacturers of the licensed and authorized COVID-19 vaccines that the COVID-19 vaccines (2024-2025 Formula) for use in the United States beginning in fall 2024 should be monovalent JN.1 vaccines.
August 2024: COVID-19 Vaccine Doses Administered Worldwide
As of 12 August 2024, 13.53 billion COVID-19 vaccine doses have been administered worldwide, with 70.6 percent of the global population having received at least one dose.
August 2024: 13.72 billion doses of COVID-19 vaccines administered worldwide
As of August 2024, 13.72 billion doses of COVID‑19 vaccines have been administered worldwide, based on official reports from national public health agencies.
October 2024: EMA Gives Positive Opinion to Update Bimervax Composition
In October 2024, the Committee for Medicinal Products for Human Use of the European Medicines Agency (EMA) gave a positive opinion to update the composition of Bimervax, a vaccine targeting the Omicron XBB.1.16 subvariant.
October 2024: US PREP Act declaration effective until October 2024
The declaration under the Public Readiness and Emergency Preparedness Act (PREP Act) effective in the United States through 1 October 2024.
May 2025: WHO recommends monovalent JN.1 or KP.2 vaccines
As of May 2025, the World Health Organization recommends that monovalent JN.1 or KP.2 vaccines remain appropriate vaccine antigens and that monovalent LP.8.1 is a suitable alternative vaccine antigen.
2026: EMA recommends updating COVID-19 vaccines to target LP.8.1
The European Medicines Agency recommends updating COVID-19 vaccines to target LP.8.1 for the 2025/2026 vaccination campaign.
Mentioned in this timeline

Ron DeSantis is an American politician who has served as...
Operation Warp Speed was a US government public-private partnership launched...

The White House located at Pennsylvania Avenue NW in Washington...
Joe Biden a member of the Democratic Party served as...
Pfizer Inc is a multinational pharmaceutical and biotechnology corporation headquartered...
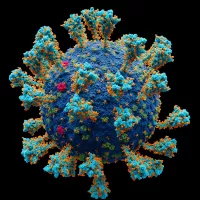
Coronaviruses are a family of RNA viruses affecting mammals and...
Trending
2 months ago Hall High School in West Hartford went into secure mode; no weapon found.

3 months ago Upstart's Q3 Earnings: Mixed Results, Soft Q4 Guidance, and Stock Slides After Announcement.
3 months ago Frank Reich Returns to Carolina, Set to Face Bill Belichick Once Again.

Penguins are flightless semi-aquatic seabirds almost exclusively inhabiting the Southern Hemisphere with the exception of the Gal pagos penguin Adapted...

2 months ago Alina Habba Disqualified: Court Rules Against Former Trump Lawyer in New Jersey Role

3 months ago Alcaraz vs Fritz Clash at ATP Finals 2025: A Minute-by-Minute Look
Popular

Thomas Douglas Homan is an American law enforcement officer who...
XXXTentacion born Jahseh Dwayne Ricardo Onfroy was a controversial yet...

William Franklin Graham III commonly known as Franklin Graham is...

Jupiter is the fifth and largest planet from the Sun...

Instagram is a photo and video-sharing social networking service owned...

Martin Luther King Jr was a pivotal leader in the...